Retinal detachment is a serious eye condition that occurs when the retina, the thin layer of tissue at the back of the eye, becomes detached from its normal position. Without prompt treatment, retinal detachment can lead to permanent vision loss. In this article, we will discuss the causes, symptoms, and treatment options for retinal detachment, with a focus on advanced treatment methods and post-treatment care.
Understanding Retinal Detachment
Retinal detachment occurs when the retina is separated from the underlying layers of the eye. This can happen due to various reasons, including trauma to the eye, age-related changes, or underlying eye conditions such as myopia or diabetic retinopathy.
Traditionally, the retinal detachment treatments involved surgery to reattach the retina to its normal position. However, advancements in technology and medical techniques have introduced newer and more advanced treatment options.
When the retina detaches, it can no longer function properly, leading to blurred or distorted vision, floaters, flashes of light, and a curtain-like effect that may gradually cover parts of your visual field.
Causes and Symptoms of Retinal Detachment
Retinal detachment can occur spontaneously or as a result of an injury to the eye. Some common causes include:
- Trauma to the eye
- Advanced age
- Eye surgery
- Eye conditions such as myopia (nearsightedness) or diabetic retinopathy
Early signs of retinal detachment may include the sudden onset of floaters, flashes of light, or a shadow or curtain-like effect in your peripheral vision. If you experience any of these symptoms, it is crucial to seek immediate medical attention, as early detection and treatment can improve the chances of restoring vision.
The Importance of Early Detection
Early detection of retinal detachment is key to preventing permanent vision loss. If left untreated, the detached retina can lose its blood supply and lead to irreversible damage to the retinal cells.
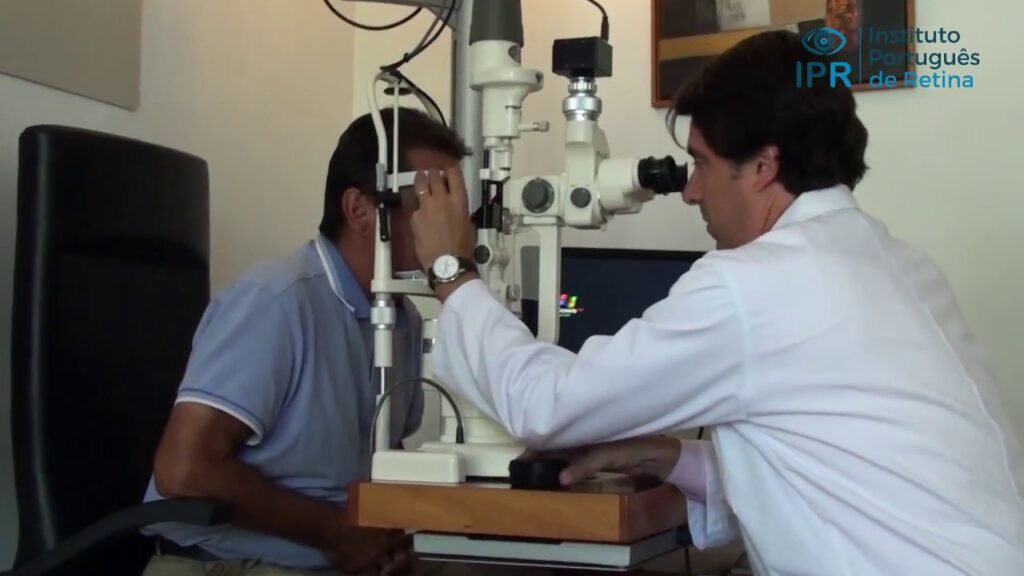
Regular eye exams play a vital role in the early detection of retinal detachment. During an eye exam, an ophthalmologist can examine the retina for any signs of detachment and recommend appropriate treatment options based on the severity of the condition.
Furthermore, it is important to note that certain individuals may be at a higher risk of developing retinal detachment. For example, people with a family history of the condition, those who have had previous eye surgeries, or individuals with a history of severe nearsightedness are more prone to experiencing retinal detachment. Understanding these risk factors can help individuals be more proactive in monitoring their eye health and seeking timely medical attention if needed.
In addition to regular eye exams, maintaining good overall eye health is crucial in reducing the risk of retinal detachment. This includes protecting the eyes from trauma, wearing appropriate eye protection during activities that pose a risk of injury, and managing underlying eye conditions such as diabetes or myopia. By taking these preventive measures, individuals can significantly lower their chances of developing retinal detachment.
Overview of Retinal Detachment Treatments
Retinal detachment is a serious condition that requires prompt treatment to prevent permanent vision loss. The retina is a thin layer of tissue located at the back of the eye that is responsible for capturing light and sending visual signals to the brain. When the retina detaches from its normal position, it can lead to a loss of vision in the affected eye.
Traditional Treatment Methods
Traditional treatment methods for retinal detachment include:
- Scleral Buckling: This surgery involves placing a silicone band around the eye to push the wall of the eye against the detached retina, helping it reattach.
- Vitrectomy: In this procedure, the vitreous gel is removed from the eye and replaced with a gas or silicone oil, which helps reposition the retina.
- Cryotherapy and Laser Photocoagulation: These techniques use extreme cold or laser heat to create scars around the detached retina, sealing it back into place.
While these traditional treatment methods have been effective in reattaching the retina and restoring vision for many patients, they can be invasive and may have associated risks and complications.
The Evolution of Retinal Detachment Treatments
Advancements in retinal detachment treatments have revolutionized the field of ophthalmology. Several innovative techniques have emerged, offering less invasive options and improved outcomes for patients.
One of the newer treatment options for retinal detachment is pneumatic retinopexy, a minimally invasive procedure that involves injecting a gas bubble into the eye to push the retina back into place. This procedure can often be performed in an office setting and may have a faster recovery time compared to traditional surgeries. Learn more about pneumatic retinopexy on https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5859893/
Advanced Treatment Options
Vitrectomy: A Modern Approach
Vitrectomy is a widely used surgery for retinal detachment, especially in complex cases. This procedure involves removing the vitreous gel, which may contain scar tissue or other substances causing the detachment. Once the vitreous gel is removed, the retina can be repositioned and secured using laser or cryotherapy techniques.
During a vitrectomy, the surgeon makes tiny incisions in the eye to access and remove the vitreous gel. Advanced microsurgical instruments are used to carefully peel away the gel and any scar tissue present. This delicate procedure allows for precise manipulation of the retina, ensuring it is properly reattached to the back of the eye.
Vitrectomy is often recommended when other less invasive treatments have not been successful or in cases where the retinal detachment is severe. The surgery is performed under local or general anesthesia, and patients may experience some discomfort and blurred vision in the days following the procedure.
Pneumatic Retinopexy: A Non-Invasive Option
Pneumatic retinopexy is a minimally invasive procedure that can be used to treat certain types of retinal detachment. During this procedure, a gas bubble is injected into the eye, which helps push the detached retina back into place. Laser or cryotherapy is then used to seal the retina in its corrected position.
Pneumatic retinopexy has the advantage of being a same-day procedure, eliminating the need for a hospital stay. However, this technique is not suitable for all retinal detachments and may require careful patient selection.
Patients undergoing pneumatic retinopexy are typically instructed to maintain a specific head position for a period of time following the procedure. This positioning helps the gas bubble exert pressure on the retina and facilitate proper reattachment. While pneumatic retinopexy can be effective for certain cases of retinal detachment, regular follow-up appointments with an eye care specialist are essential to monitor the healing process and ensure the long-term success of the treatment. Click here to read more about healing process.
Post-Treatment Care and Recovery
After retinal detachment treatment, it is essential to follow the prescribed post-operative care instructions to promote healing and prevent complications. These may include:
What to Expect After Treatment
- Wearing an eye patch or shield
- Using prescribed eye drops or medications
- Avoiding strenuous activities or heavy lifting
- Sleeping with your head elevated
Your ophthalmologist will closely monitor your progress and schedule follow-up appointments to ensure that your eye is healing properly.

Tips for a Smooth Recovery
During the recovery period, it is important to take certain precautions to support the healing process. These may include:
- Avoiding rubbing or touching the treated eye
- Avoiding activities that may increase eye pressure, such as bending or straining
- Eating a balanced diet rich in vitamins and minerals to support eye health
- Wearing protective eyewear in bright sunlight or hazardous environments
Additionally, it is recommended to avoid smoking and limit alcohol consumption during the recovery period, as these habits can impede the healing process and increase the risk of complications. Adequate rest and sleep are crucial for allowing your body to recover effectively and for promoting overall well-being.
Emotional Support During Recovery
Recovering from retinal detachment treatment can be a challenging time both physically and emotionally. It is normal to experience a range of emotions, including anxiety, frustration, or fear about the outcome of the treatment. Seeking support from friends, family, or a mental health professional can help you navigate these feelings and maintain a positive outlook during your recovery.
Preventing Retinal Detachment
While not all cases of retinal detachment can be prevented, there are steps you can take to reduce the risk:
Regular Eye Exams: A Key to Prevention
Scheduling regular eye exams with an ophthalmologist is crucial for maintaining eye health and detecting early signs of retinal detachment. Your eye doctor can assess your risk factors and recommend appropriate preventive measures.
Lifestyle Changes to Reduce Risk
In some cases, retinal detachment can be caused or exacerbated by factors such as severe myopia or high blood pressure. Making lifestyle changes, such as wearing prescribed eyeglasses or contacts and managing hypertension, can help reduce your risk of developing retinal detachment.
Moreover, maintaining a healthy diet rich in antioxidants and omega-3 fatty acids can also play a role in preventing retinal detachment. Foods like leafy greens, fish, nuts, and seeds can help support eye health and reduce inflammation, potentially lowering the risk of detachment.
Additionally, avoiding activities that pose a high risk of eye injury, such as contact sports without protective eyewear, can also contribute to preventing retinal detachment. Protecting your eyes from trauma is essential in safeguarding the delicate structures within the eye, including the retina.
Learn more about retinal damage symptom on: Symptoms of Retinal Damage